By ADMIN on September 06, 2017

By ADMIN on May 14, 2015
Cognitive Behavioral Therapy: Treating the mind as it relates to chronic pain
Ever wonder why some people experience chronic pain? Why some people seem to recover from an injury within weeks while others continue to experience symptoms months or even years after? Chronic pain is defined as any persistence of pain beyond three months duration. There are many factors, both physical and psychological, that affect whether a person will feel pain and how long that pain will last.
In the case of an acute injury, the intensity of pain typically correlates to the degree of damage/injury to the body. In 1965, Melzak and Wall described the Gait Control Theory of pain. According to this theory, once sensed by our peripheral nervous system, a noxious stimulus must pass through the spinal cord and up to the brain to be interpreted as “painful.”
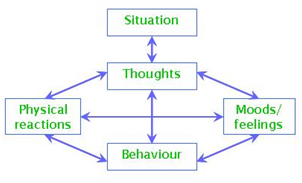
Just like physical stimuli, thoughts and behaviours have the capacity to open/close the gait, thereby amplifying or dampening the pain. Cognitive behavioural therapy (CBT), begins with the premise that maladaptive beliefs and behaviours play an important role in the maintenance or exacerbation or mood, anxiety and somatic problems. People have beliefs, coping deficits and behavioural responses which make sense in situations involving acute pain but which become problematic in cases involving prolonged pain. An Athlete’s Care chiropractor trained in CBT principles can work with the patient to bring these thought patterns to the surface to determine whether the patients’ reactions to situations are accurate.

Through CBT, thoughts and beliefs are categorized into 3 levels : Automatic thoughts, intermediate beliefs and core beliefs. Automatic thoughts are at the surface (most easily accessible), are typically specific to a situation, and are most changeable. Core beliefs are deeply rooted views we have about ourselves and the world. They are general statements. These are least changeable and we are often not conscious of these core beliefs. Intermediate beliefs are the level in between.
Automatic thoughts - Intermediate beliefs - Core beliefs
Consider an example scenario: you are waiting to meet a friend for lunch in a restaurant and they are a half hour late
|
Interpretation |
1 |
2 |
3 |
|
Automatic thought |
They’ve been in an accident. |
They don’t want to have lunch with me. |
How rude. They always pull stuff like this. |
|
Intermediate belief |
They may be really hurt |
People don’t want to be my friend |
They are not respectful of my time |
|
Core belief |
People are susceptible to leaving/dying |
I am not loveable |
People will hurt me/disrespect me |
|
Bodily reaction/behaviour |
sweating, quickened heart beat, fidgeting, looking around, checking cell phone
|
hunched over, dejected and depressed
|
increased blood pressure, tension in upper traps, neck/back à muscle/joint pain
|
The above example highlights the various ways the mind and body can respond based on automatic thoughts that arise in a given situation. The resultant bodily reactions and behaviours can be quite different depending on the person’s internal thoughts and interpretation of the scenario.
As Athlete’s Care chiropractors, we are trained in functional integrated therapy, patient-centered care and holistic health. Often times with chronic pain, maladaptive thoughts and subsequent behaviours can keep a patient in the cycle of chronic pain, thereby preventing full recovery. By examining and challenging these thoughts using CBT principles, one can change the resulting behaviour, thereby affecting the sensation of pain.
Dr. Pamela MacDonald is a chiropractor currently seeing patients at Athlete's Care in the Beach and at the new clinic in Etobicoke/Kingsway.
... moreBy ADMIN on March 17, 2015
By Dr. Amanda Scione DC., B.Sc Kin.

Have you ever been performing an activity and then wake up the next day in pain…leaving yourself wondering what you did to yourself to cause this? Or how about when the pain is not going away despite treatment to the area?Have you ever wondered why therapists treat adjacent regions of your body that are not necessarily painful?
Answers to these questions will be illustrated by explaining the principles of the joint by joint approach, how pain in one area may be caused by dysfunction in another, and how these issues can be resolved.
Whether you engage in moderate or intense physical activity it is important for you to understand the following concepts. As a patient, it is important to understand the basics of how your body functions. This will make you more in tune with your body, and will allow you to feel when something is ‘not right’. The Joint by Joint Approach was coined by Michael Boyle and Gray Cook. Their analysis of the body is very straightforward. Our bodies are merely seen as a stack of joints. Each joint or series of joints has a specific function, and therefore, has particular training needs. Notice below that our joints alternate between mobility and stability.

If the specific functions of each joint are not met, our bodies are prone to predictable levels of dysfunction. Problems at one joint usually show up as pain in the joint above or below. Let’s use the common condition of lower back pain to illustrate this. I am sure you know by now that if you have lower back pain you need to work on your core exercises. BUT, what you may not know is that this lower back pain probably evolved due to a loss of hip mobility. As we previously discussed, when we have loss of function in one joint (lower spine), we also get loss of function of the joint below (the hips). This means that if the lumbar spine can not move, the hips will instead. The problem is that the hips are designed for mobility, and the lumbar spine for stability. When the intended mobile joint becomes immobile, the stable joint is forced to move as compensation, becoming less stable and subsequently painful.
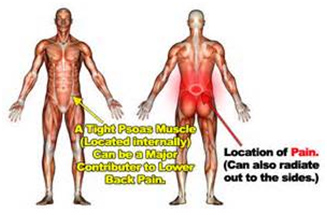
Let’s analyze this pattern further. As shown in the diagram, decreased strength or activation of the psoas muscle will cause patterns of lumbar flexion as a substitute for hip flexion. Decreased strength or activation of the glut muscles will cause a compensatory extension pattern of the lumbar spine to replace the motion of hip extension. This cycle is a vicious one. As the spine moves to compensate for the lack of strength and mobility of the hip, the hip loses more mobility.
Quick Summary of patterns:
Loss of ankle mobility » knee pain
Loss of hip mobility » low back pain
Loss thoracic mobility » neck and shoulder pain, or low back pain

Remember that the chain starts from the bottom. An immobile ankle causes the stress of landing to be transferred to the joint above, the knee- and the cycle continues up.
Utilizing the FIT principle, the chiropractors at Athlete’s Care are equipped in identifying these patterns of altered joint mechanics as well as correcting them through many different treatment strategies. We find and treat the cause of the pain rather than focus on the source of the pain. Elite athletes utilize this approach for performance optimization. They are constantly assessed for altered joint mechanics BEFORE compensation and pain sets in. Visit your nearest chiropractor at Athlete’s Care to get your body assessed now!
Dr. Amanda Scione is a chiropractor currently seeing patients at the Athlete’s Care Oakville location. Wait for upcoming news on the Hamilton location.
... moreBy ADMIN on July 16, 2014
Dr. Trevor Vander Doelen was recently interviewed by a CrossFit athlete about his approach to care for CrossFit athletes, injury prevention, and improving performance.
To what do you attribute your success in treating CrossFit athletes and getting them back to their sport both pain free and performing at a higher level?
CrossFit is an incredible sport that combines strength, stamina, and skill and every athlete has their own particular strengths and weaknesses. Similarly, all CrossFit athletes need an individualized approach to their care when they are injured. Every athlete is at a different level of movement quality, strength, and body awareness and as such needs to be treated differently.
The foundation of my approach involves not just treating pain but more importantly correcting dysfunctional movement patterns.
A thorough initial assessment involving a detailed history of current and past injuries as well as a movement-based assessment is an essential starting point for each athlete. Once movement dysfunction is determined, a detailed plan of how to correct this is discussed with the patient. Treatment predominantly involves Active Release Technique (ART), joint manipulation, and neurofunctional acupuncture, followed by a specific and progressive corrective exercise plan.
What should I include in my warm up and cool down?
Static stretching prior to exercise has been shown to hinder performance in explosive sports and therefore should be avoided prior to a CrossFit workout. However dynamic stretches to “prime” the nervous system should be done prior to exercise. These should include active movements of the ankles, knees, hips, spine, shoulders, elbows, and wrists in all planes of motion prior to starting the workout.
Low back pain seems to be very common amongst the Cross-Fit community, what steps can I take to prevent low back pain?
You are correct, many injured CrossFit athletes present with low back pain. Anecdotally, I find the main culprit with acute low back pain amongst these athletes is the deadlift and squat exercise. These exercises, when performed with correct posture, are great movements for functional core strength, hip strength, and shoulder strength. With that being said, when these exercises are performed without a neutral spine and without a good hip hinge it is only a matter of time before the athlete loads to the point of injury. My movement assessment is able to determine why an athlete moves poorly. As an example, I often find the core and gluteal muscles are inhibited (underactive) by facilitated (overactive) hip flexors amongst these athletes. Manual therapy and movement correction are very effective at helping these athletes recover and prevent this low back pain from returning in the future.
How can I minimize shoulder problems?
Unfortunately if you have had shoulder problems in the past, the likelihood of recurrence is increased. It is important to get the shoulder assessed by a health care professional that uses a movement-based assessment.
Since the shoulder blade is attached to the ribcage and mid back by soft tissue structures (muscle and fascia) it responds very well to manual therapy, acupuncture, and corrective exercise. Typical shoulder injuries with CrossFit athletes involve subacromial and posterior internal impingement. Most of these athletes have facilitated (overactive) pectoral and upper trapezius muscles and inhibited (underactive) lattisimus dorsi and middle/lower trapezius muscles. This prevents them from keeping their arm and shoulder blade in the proper position during movement. While this is a typical presentation, I must emphasize again that no two patients are identical in their presentation; I often see dysfunctional core stability and hip mechanics with these same athletes.
Addressing these dysfunctions through specific stability and mobility corrective exercises, a CrossFit athlete can effectively prevent shoulder pain.
How can I improve my squat?
This is a common question that I get asked frequently from the CrossFit community. The best answer to this question is to get assessed by a Certified Strength and Conditioning Specialist (CSCS) or Chiropractor with a movement based assessment that has experience working with olympic lifting, power lifting, or CrossFit.
I often address this movement dysfunction by comparing the body to a computer with a hardware vs. software analogy. The athlete requires stability and mobility from various joints and soft tissues surrounding them (hardware) and also requires efficient and safe movement driven by the nervous system (software).
When assessing the “hardware” component I often reference legendary strength coach Mike Boyle’s joint-by-joint approach that states that certain joints tend towards certain types of dysfunction. Often the foot, knee, lumbar spine, cervical spine, and scapulothoracic joint have lost stability, and the ankle, hip, thoracic spine, and glenohumeral joint have lost mobility.
Dysfunctional “hardware” responds well to corrective exercise and even better to corrective exercise in combination with manual therapy.
A “software” assessment focuses on the athlete’s technique, body position, and muscle activation patterns and will provides feedback on the athlete’s specific approach to the movement. Modifying key factors like specific joint positions, and activation from the feet, through the hips, into the core, and shoulders helps create movement awareness and efficiency with the movement.
Once the efficiency of the athlete’s squat movement has improved, the athlete can then progressively load their squat. This whole-body approach to squat correction prevents the most common issues with the movement, including low back pain, wrist pain in the front rack position, and allows for greater depth. This is the best way to make long-term changes to your squat for both injury prevention and performance.
To summarize our interview, what last piece of advice would you give a CrossFit athlete who is interested in injury prevention and performance in this great sport?
Empower yourself! Injury prevention and performance in this sport is completely within your control. Take an active approach to learning about your body by putting together a team of training and health care professionals that can both help you and teach you to help yourself safely and efficiently get faster and stronger for longer.
Dr. Trevor Vander Doelen is a movement-based Chiropractor at Athlete's Care in Liberty Village, that helps recreational, amateur, and professional athletes perform better and return to their sport following injury.
... moreBy ADMIN on July 03, 2014
It was early October and I was on my way to the airport, looking forward to 7 days of sun and surfing in Brazil. As per the usual arrangement, I presented my passport at the Air Canada desk, only to hear, we don’t have a ticket for you Mr. Klachan. As it turns out, the travel agent made the ticket for Christopher David, not Christopher David Klachan, which in the eyes of Air Canada is a different person. After an hour of trying to keep my calm while ‘politely discussing’ with the Air Canada staff, I realized I wasn’t going anywhere. It would have been useful to know at the time, that this would ultimately take me to the Winter Olympics in Sochi to work with a number of the US bobsled and skeleton team.
Two days later, I received an email from Dr. Mark Scappitticci and Dr. Mike Prebeg explaining that a two time Summer Olympic medalist was looking for therapy to help her prepare for the US Olympic Trials in bobsleigh. I had worked with bobsledders before, but the thought of working with a winter sport made me slightly resent missing my trip to Brazil. At the same time, I had heard nothing but great things about working with this athlete so I thought I would give it a go.
 I spent 4 days working with a number of athletes, most of whom were selected to represent the US on the World Cup Tour. A couple weeks later, they asked if I could help out with a World Cup event in Park City, Utah. After a successful double header in Utah, they asked if I would join them for three weeks in Europe on the World Cup. As time passed, a number of athletes were added to the treatment roster, and when US Olympic team was selected at the near end of the World Cup season, all of the athletes I was working with made the team. At the end of the World Cup season, the US women’s bobsled were sitting in 2nd, 3rd and 7th going into the Olympics and the athletes and coaches started discussing the potential of me joining them in Sochi. To my great surprise, the US Olympic Committee was able to arrange a visa, flight and accreditation in the last few days prior to the opening ceremonies. Forty-eight hours later I was heading up the gondola to the Sochi Mountain Village to work out of US sports medicine.
I spent 4 days working with a number of athletes, most of whom were selected to represent the US on the World Cup Tour. A couple weeks later, they asked if I could help out with a World Cup event in Park City, Utah. After a successful double header in Utah, they asked if I would join them for three weeks in Europe on the World Cup. As time passed, a number of athletes were added to the treatment roster, and when US Olympic team was selected at the near end of the World Cup season, all of the athletes I was working with made the team. At the end of the World Cup season, the US women’s bobsled were sitting in 2nd, 3rd and 7th going into the Olympics and the athletes and coaches started discussing the potential of me joining them in Sochi. To my great surprise, the US Olympic Committee was able to arrange a visa, flight and accreditation in the last few days prior to the opening ceremonies. Forty-eight hours later I was heading up the gondola to the Sochi Mountain Village to work out of US sports medicine.
A day in the life
Success in both bobsled and skeleton is largely dependent on the athletes being able to accelerate the sleds from a dead start. All driving being equal, the athlete with the fastest start time, producing the greatest start velocity, will win the event. Essentially, the athletes are powerful sprinters that have perfected a way to ‘hit’ the sled with enormous power and accelerate it to maximum velocity.
Whether it was training day or race day, most of the athletes received a pre performance treatment. These treatments were aimed at optimizing joint mechanics, muscle tension and force production, mostly utilizing soft tissue work, performance taping, mobilization and manipulation. After training had finished, a more thorough treatment was administered to work with any nagging injuries or simply to further the optimization process. Regardless of the objective, the athletes were assessed functionally and orthopedically, using range of motion, manual muscle testing, movement screens and other. Stuart McMillan, a very successful sprint and push coach was enormously useful in providing information on functional deficits to search for based on slow motion video analysis and his inspection of the athletes during warm up, training and racing. Based on the findings, a combination of electro-acupuncture, soft tissue work, joint mobilization/manipulation and performance taping was again administered. A number of other staff members working with sports medicine were wondering why the athletes were treated so frequently. I explained that the objective was to catch something before it progressed to a more significant issue. If we were to recognize an inhibited muscle necessary to performance, we would aim to facilitate it before the athlete created a work around motor program that was more metabolically, neurologically or mechanically taxing.
On tour, some injuries require a little more attention than others. A bobsleigh drivers had experienced a couple of crashes in training going into the Olympic final. The crashes had left the athlete with not only strained neck muscles but an agitated neurological state. In this case, as much focus was placed on restoring sympathetic-parasympathetic nervous system balance as it was addressing the physical injuries. A little fight or flight is good for a short duration but this athlete had to be in a good head space to keep their muscle tone in the right spot and to stay calm and focussed while weaving a bobsleigh at close to 150 km/h. Dry needling or acupuncture was again used to facilitate this process.
 An athlete’s worst nightmare, you’re in your second of four heats, on your first of two days of competition and you feel a pop in your calf when accelerating. To top it off, you are sitting in medal contention and you still have one more event to compete in five days later. Do you drop out and save it for the next competition, do you go 50% and fall out of medal contention. The beauty of the human body is that redundancy is often built in. In this case the athlete was fortunate in that the compromised tissue is one of six that can help perform the roll of ankle plantar flexion and he was up for the battle. It was determined that the bottom of the inner gastrocnemius where it meets with the upper achilles tendon had been partially torn, furthermore, inhibition in his gluteus maximus was found. The approach was to facilitate the healing of the torn tissue, while to simultaneously ensure the other muscles assisting in the kinetic chain of hip, knee and ankle extension were not inhibited. The motor points of the assisting muscles were all stimulated with electro-acupuncture along with the trunk of the tibial nerve. Simultaneously, gentle soft tissue was administered above and below the injured site in an attempt to not let the adjacent soft tissue recoil away. Finally, to facilitate the assisting muscles and protect the injured tissue performance taping was administered. It wasn’t perfect, but the result was he was able to maintain his bronze position on day two and push to another bronze in four man a few days later at a self proclaimed 95%.
An athlete’s worst nightmare, you’re in your second of four heats, on your first of two days of competition and you feel a pop in your calf when accelerating. To top it off, you are sitting in medal contention and you still have one more event to compete in five days later. Do you drop out and save it for the next competition, do you go 50% and fall out of medal contention. The beauty of the human body is that redundancy is often built in. In this case the athlete was fortunate in that the compromised tissue is one of six that can help perform the roll of ankle plantar flexion and he was up for the battle. It was determined that the bottom of the inner gastrocnemius where it meets with the upper achilles tendon had been partially torn, furthermore, inhibition in his gluteus maximus was found. The approach was to facilitate the healing of the torn tissue, while to simultaneously ensure the other muscles assisting in the kinetic chain of hip, knee and ankle extension were not inhibited. The motor points of the assisting muscles were all stimulated with electro-acupuncture along with the trunk of the tibial nerve. Simultaneously, gentle soft tissue was administered above and below the injured site in an attempt to not let the adjacent soft tissue recoil away. Finally, to facilitate the assisting muscles and protect the injured tissue performance taping was administered. It wasn’t perfect, but the result was he was able to maintain his bronze position on day two and push to another bronze in four man a few days later at a self proclaimed 95%.
All in all, the athlete is able to appraise the outcome of the treatments almost immediately after and in sport there are numbers to confirm or deny. In day-to-day injuries, a patient may not have the objective data, but the approach is still driven by the same understanding of anatomy, neurology and physiology. The end result may be as simple as a patient who suffered a strain in the office, can now comfortably sip his caipirinha on the beach in Brazil.
Christopher Klachan, DC, BSc, CSCS, is currently seeing patients at two downtown Toronto locations, Athlete's Care Sports Medicine Centre in Yorkville and at Adelaide and York.
... more